Diverticulitis: Causes, Symptoms and Natural Support Strategies
Diverticulitis is a condition that affects the colon and is becoming increasingly common, especially in Western societies. From a functional medicine perspective, we don’t just treat symptoms, we look deeper to understand why the body is struggling in the first place.
Our goal is to support healing at the root level by restoring balance in the gut, reducing inflammation, and strengthening the body’s natural defences.
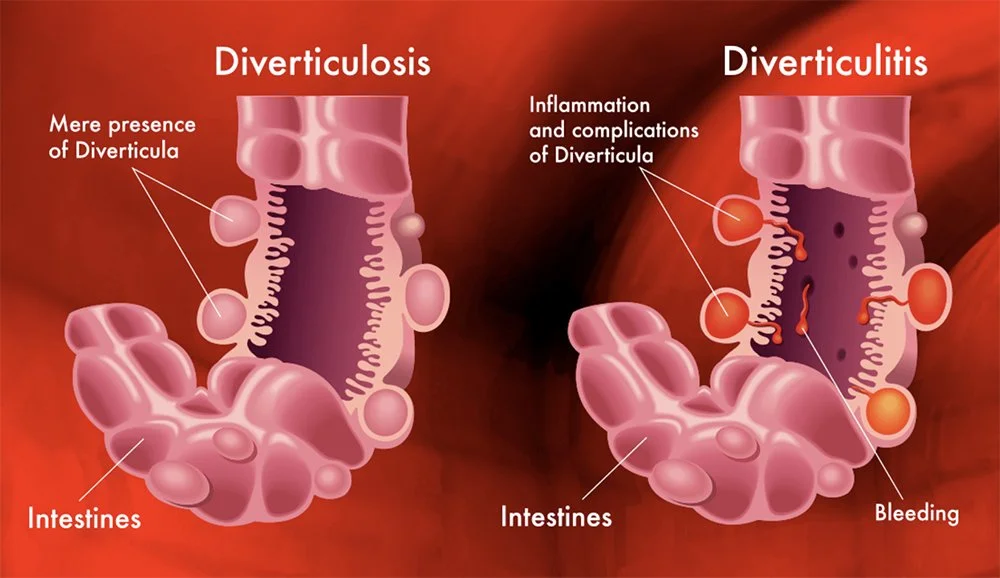
What Is Diverticulitis
Diverticulitis occurs when small pouches called diverticula, which form in the wall of the colon, become inflamed or infected. These pouches are often silent and cause no problems until irritation or infection sets in. When that happens, people often experience symptoms such as abdominal pain, most commonly on the lower left side, bloating, cramping, and changes in bowel habits like constipation or diarrhoea. In more acute cases, fever, nausea, and fatigue can occur, making it a painful and disruptive condition.
Root Causes from a Functional Medicine Perspective
Rather than focusing only on the pouches themselves, functional medicine looks at why the colon is under stress in the first place. Some of the deeper imbalances that may contribute to diverticulitis include poor gut motility, low dietary fiber, an unhealthy gut microbiome, chronic inflammation, food sensitivities, and weak digestive function. Liver congestion and inadequate bile flow can also play a hidden but powerful role, as they affect how well we digest fats and detoxify waste, both of which are vital for colon health.
Natural Gut Support and Healing
Supporting the gut lining and reducing inflammation are essential steps in healing diverticulitis. One of the most effective nutrients for this is L-glutamine, an amino acid that helps repair and strengthen the intestinal lining. Another powerful gut healer is larch arabinogalactan, a type of prebiotic fiber that nourishes beneficial bacteria and supports the immune system in the gut.
Vitamins D and A are also crucial, as both play a role in immune regulation and help maintain the integrity of the gut lining. When these vitamins are deficient, the gut is more vulnerable to irritation and infection. Zinc carnosine offers further support by enhancing mucosal repair, while aloe vera can help soothe and calm inflamed tissues. For managing inflammation, boswellia, a resin used traditionally in Ayurvedic medicine, has been shown to help reduce inflammatory processes in the gut.
Rebalancing the Microbiome with the Right Probiotic
The health of the microbiome plays a vital role in both the onset and resolution of diverticulitis. When the balance of bacteria in the colon is disrupted, known as dysbiosis, harmful bacteria can take over, leading to inflammation, bloating, and infection. Restoring microbial balance is a key goal in functional medicine.
Probiotics can help reintroduce beneficial bacteria and support the gut’s natural defenses. For individuals sensitive to fermented foods or who experience reactions like itching, fatigue, or bloating, a low-histamine probiotic may be the best option. These formulations avoid strains known to produce or release histamine, which can worsen inflammation in some sensitive people. Another well-tolerated option is spore-based probiotics (sporebiotics), which are more resilient to stomach acid and antibiotics, and work by creating a healthy environment that encourages native beneficial bacteria to thrive.
In some cases, probiotics alone aren’t enough, especially when there is active infection or overgrowth of harmful microbes. Antimicrobial herbs can be used alongside probiotics to help reduce the load of pathogenic bacteria. Berberine, found in herbs like goldenseal and Oregon grape, is a powerful natural antimicrobial that can target unwanted bacteria without harming the beneficial strains. Garlic extract, particularly in its aged or allicin-rich form, also offers strong antimicrobial effects and helps fight infection while supporting immune function. These can be used for a short period as part of a gut restoration protocol and followed with gut-healing nutrients and a tailored probiotic plan.
The Liver–Colon Connection
The liver plays a central role in digestion and detoxification, and its health directly influences the colon. When liver function is sluggish, bile production may be reduced. Bile is essential not just for digesting fats, but also for keeping the colon clean, antimicrobial, and moving regularly. Poor bile flow can lead to constipation, bacterial overgrowth, and irritation in the colon.
To support liver health and bile flow, we can use bitter foods like dandelion greens, arugula, and lemon. Herbal extracts such as milk thistle and artichoke can help stimulate liver detoxification.
One particularly important nutrient here is phosphatidylcholine, which supports both bile fluidity and the integrity of cell membranes throughout the body, including in the liver and gut lining.
Methylation: The Detox Engine
Methylation is a process your body uses to manage toxins, regulate genes, and balance neurotransmitters and histamine levels. When methylation is sluggish, due to nutrient deficiencies, genetics, or chronic stress, the body can’t detoxify properly, and inflammation can build up.
Key nutrients that support healthy methylation include B12, folate (vitamin B9), B6, and magnesium. These are often depleted in people with digestive issues or high stress levels. Supporting methylation not only improves liver function but also helps with histamine detoxification, which can reduce reactivity and inflammation in the gut.
Reducing Inflammation and Rebuilding Tissues
Inflammation plays a major role in diverticulitis, so calming the immune response is critical. Omega-3 fatty acids from fish oil or algae can help reduce inflammation throughout the body, including the gut and liver. These healthy fats also strengthen cell membranes, making them more resilient to damage.
Curcumin, the active compound in turmeric, is another powerful anti-inflammatory that supports gut lining repair and immune balance. For some people, collagen peptides can also be helpful. Collagen provides amino acids like glycine and proline, which are needed for gut lining repair and connective tissue strength.
Lifestyle Changes That Matter
Healing the gut goes beyond supplements. Diet and lifestyle form the foundation of functional healing. Eating a variety of whole, fibre-rich plant foods can support regular bowel movements and feed good gut bacteria, though during a diverticulitis flare, a gentler, low-fibre approach may be necessary until inflammation calms down.
Hydration is essential to help fibre work effectively and support detoxification.
Movement is another important piece. Gentle exercise like walking, stretching, or yoga encourages bowel motility and reduces stress. Managing stress through breathwork, meditation, or therapy can have a significant impact on gut health, since stress slows digestion and increases inflammation. Avoiding processed foods, sugar, and alcohol is also key to reducing strain on both the gut and the liver.
Putting It All Together
Diverticulitis doesn’t occur in isolation, it’s a sign that your digestive system, and possibly your detox pathways, need extra support. From a functional medicine viewpoint, this means working with your body, using nutrients and herbs that promote healing, and creating a lifestyle that supports long-term balance.
By addressing root causes like inflammation, microbial imbalances, poor bile flow, and weakened gut lining, we can create the conditions for true healing.
Everyone’s journey is unique, so consider working with a functional medicine practitioner who can help tailor a plan to your body’s specific needs.